Índice
¿Qué es la hipoxia estancada y por qué importan los segundos?
La hipoxia estancada se produce cuando la sangre rica en oxígeno se estanca antes de poder nutrir los órganos vitales, normalmente durante un shock, una insuficiencia cardiaca congestiva o coágulos venosos profundos. Las autoridades médicas la agrupan en cuatro cuadros clásicos tipos de hipoxiaPero sólo la hipoxia estancada comienza con un colapso circulatorio, no respiratorio, lo que significa que el oxígeno suplementario por sí solo no puede salvar el tejido. Los libros de texto de fisiología señalan que incluso una breve pérdida de flujo provoca inanición en las células cerebrales, mientras que los ensayos muestran que la hipoperfusión sistémica duplica la mortalidad si la reperfusión supera los 30 minutos. Dado que la ventana de peligro es corta, los servicios de urgencias de Florida deben clasificar inmediatamente los indicadores de shock o arriesgarse a sufrir lesiones catastróficas.
Causas ocultas que los médicos deben detectar antes de que mueran los tejidos
El shock cardiogénico tras un infarto, el shock séptico por infección, el shock hipovolémico tras un traumatismo y la isquemia localizada por torniquetes o síndrome compartimental de las extremidades cortan el flujo sanguíneo regional y provocan hipoxia estancada. Los manuales de cuidados críticos citan las extremidades frías y húmedas, la presión de pulso estrecha y el descenso de la diuresis como señales de colapso circulatorio que obligan a administrar líquidos o vasopresores en cuestión de minutos. No volver a conectar una vía de presión, ignorar un catéter central ocluido o retrasar la fasciotomía pueden prolongar los estados de bajo flujo, permitiendo que se instale la acidosis celular, un escenario que Percy Martinez comprueba rutinariamente con los datos de la historia clínica y los registros del monitor de cabecera.
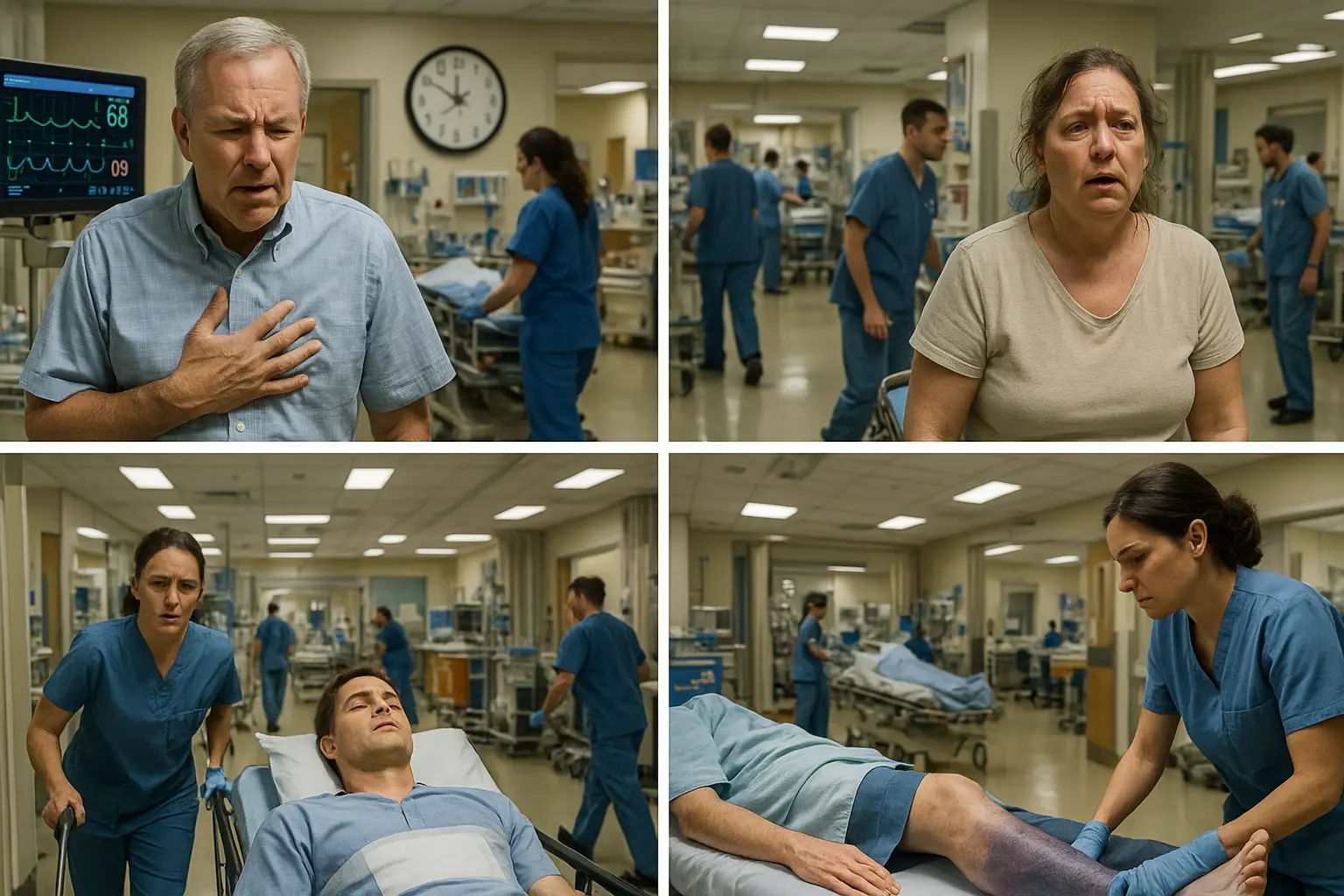
Los primeros síntomas suelen ser percibidos por las familias
Los pacientes se muestran agitados, confusos o inusualmente somnolientos a medida que desciende la perfusión cerebral; la piel se vuelve pálida, moteada o cianótica; los dedos se sienten helados a pesar de la temperatura ambiente cálida; y la diuresis desciende por debajo de 0,5 ml/kg/hora. Las publicaciones sobre urgencias confirman que estas señales visibles aparecen antes del colapso cardíaco completo, lo que ofrece una ventana de diagnóstico crítica que el personal ocupado a veces pasa por alto. Los seres queridos que alertan a las enfermeras pero no reciben una evaluación rápida deben documentar cada solicitud; ese registro a menudo se convierte en una prueba clave cuando Percy Martínez reconstruye la cronología de las alarmas omitidas en un tribunal.
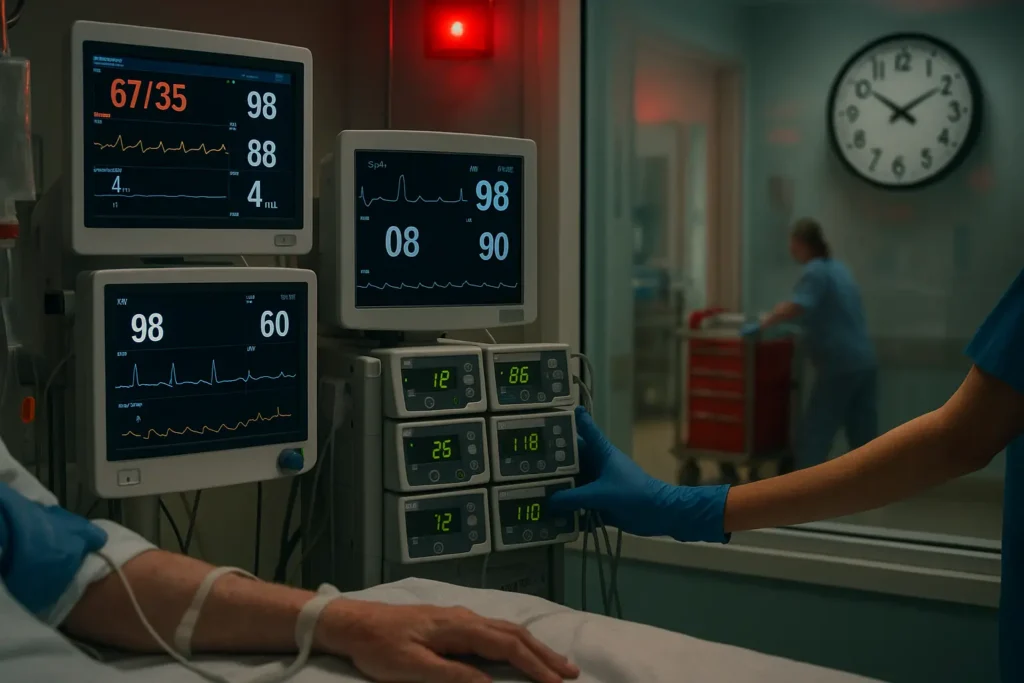
Cómo deben confirmar los hospitales la hipoxia estancada en minutos
Los cuidados estándar exigen la realización simultánea de pulsioximetría, gasometría arterial, lactato sérico, ecocardiografía a pie de cama y angiografía Doppler o TC cuando se sospecha isquemia de las extremidades. Directrices mostrar elevado El lactato y el descenso de la saturación venosa mixta de O₂ indican hipoperfusión sistémica incluso cuando la SpO₂ es normal. La ecografía en el punto de atención señala un taponamiento o un coágulo masivo en diez minutos. Los intensivistas de Percy Martínez comprueban si estos estudios se solicitaron y se realizaron con la suficiente rapidez; cualquier laguna inexplicable puede dar lugar a una demanda por negligencia.
El tratamiento adecuado restablece el flujo: la demora abre la puerta a la mala praxis
La terapia basada en la evidencia combina fluidos isotónicos agresivos, vasopresores, inotrópicos, revascularización o fasciotomía emergente con oxígeno controlado y manejo de la temperatura. Los textos de cardiología advierten de que cada 10 minutos de retraso en el restablecimiento de la presión arterial media por encima de 65 mmHg aumenta el riesgo de fallo multiorgánico en un 7%. Cuando los equipos esperan a la obtención de imágenes electivas, descuidan la titulación de los presores o programan mal las bombas de infusión, la hipoxia estancada se convierte en anoxia irreversible, motivo de veredictos de ocho cifras que Percy Martínez ha conseguido de las principales aseguradoras hospitalarias de Florida.
| Condición desencadenante | Error médico típico |
|---|---|
| Shock cardiogénico post IM | Retraso en el inicio de los vasopresores |
| Shock séptico | Antibióticos tardíos de amplio espectro |
| Síndrome compartimental | Presiones compartimentales omitidas |
| Uso del torniquete en cirugía | Superación de los límites de seguridad |
| Embolia pulmonar | No solicitar una angiografía por TC |
¿Cuándo un retraso hospitalario se convierte en falta legal en Florida?
En virtud del artículo 766.106 de los Estatutos de Florida, las víctimas disponen de dos años a partir de la presentación de la prueba y deben presentar un escrito detallado en el que se especifiquen los motivos de la infracción. notificación previa a la demanda, pero una monitorización negligente que prolongue la hipoxia estancada puede ampliar la responsabilidad más allá de los límites habituales, ya que los daños no económicos ahora no tienen límite y las pérdidas económicas son ilimitadas. Las tendencias de los jurados muestran indemnizaciones multimillonarias por hipoxia no tratada en recién nacidos ($2,5 millones, 2017) y adultos ($11 millones, 2023) una vez que el abogado demuestra las infracciones del protocolo. Percy Martínez presenta citaciones para formas de onda de monitores, metadatos de HCE y registros de personal en cuestión de días para bloquear las pruebas antes de que los hospitales puedan purgar las copias de seguridad rotativas, una táctica que convierte la fisiología compleja en una clara negligencia legal.
Resultados probados de Percy Martínez en litigios por hipoxia
Nuestra firma aseguró acuerdos confidenciales de ocho cifras para un amputado de Tampa cuyo síndrome compartimental no fue monitorizado durante seis horas y para un paciente cardíaco de Miami cuyo goteo de vasopresor se agotó. Uniendo a intensivistas certificados con ingenieros biomédicos, Percy Martínez reconstruyó minuto a minuto las lagunas de perfusión que la defensa no pudo refutar. El mismo flujo de trabajo sustenta ahora las investigaciones en todo el estado, dando a las familias ventaja para exigir los costes de atención de por vida, lucro cesante y daños por dolor sin límite, a menudo dentro de los 18 meses de la presentación.
Su auditoría legal gratuita: Próximos pasos para las familias de Florida
Llame hoy mismo y un abogado bilingüe recopilará registros, fotografiará miembros y revisará los datos del monitor en un plazo de 48 horas sin coste alguno. A continuación, entregar una matriz de responsabilidad, valoración de daños, y la línea de tiempo antes de la demanda para que sepa exactamente quién va a pagar y cómo vamos a mantener los fondos de liquidación de auditoría listo y gravamen compatible. Nuestros honorarios de contingencia significan que usted no debe nada a menos que nos recuperemos, y cada dólar económico va directamente a gastos médicos y de manutención. Sirviendo a las víctimas en toda la Florida, Percy Martínez convierte la hipoxia estancada de asesino silencioso en una historia convincente en la corte que gana una compensación que cambia la vida.
¿Necesita respuestas rápidas? Solicite su auditoría de salud legal gratuita ahora: Percy Martínez está listo para restablecer la vía de oxígeno de su familia a la justicia.