Important: This is general information for families in Florida. It isn’t medical advice. If your loved one has a rapidly worsening wound, fever, confusion, or severe pain, seek medical care immediately.
Table of Contents
When a pressure ulcer reaches Stage 4, the wound extends through skin and soft tissue and may expose muscle, tendon, or bone. It’s scary to see. In Florida long term care settings, good outcomes hinge on a consistent plan: relieve pressure, remove dead tissue, control infection, choose the right dressings, maintain nutrition, and treat pain with dignity. This guide walks you through each step, the reality of stage 4 pressure ulcer healing time, and how to spot warning signs of poor care.

What “Stage 4” means, and what families in Florida should expect
A Stage 4 wound is deep and serious. In nursing homes and hospitals across Florida, families should see a written plan that covers offloading, dressing changes, and specialist referrals. Communication matters just as much as the products used. You should understand who is doing what, and how progress will be measured week to week.
Treatment, in plain language
Offloading comes first. No treatment works if pressure isn’t removed. Your loved one should be positioned on a schedule, with a surface that redistributes weight and heel protection when needed. Ask staff to show you the turning plan and how it’s documented each shift.
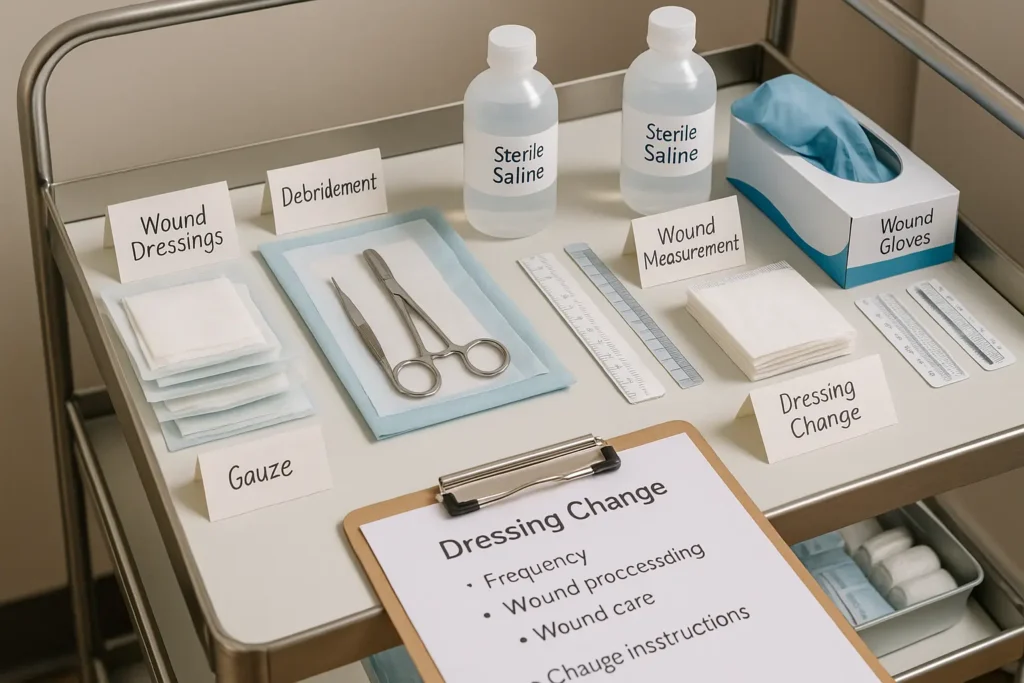
Debridement clears the way. Dead tissue blocks healing. The team may use sharp, enzymatic, autolytic, or mechanical methods depending on the wound. You don’t need to become a clinician, just ask which approach is being used and why.
Infection control protects progress. Deeper wounds carry higher infection risk. The plan might include cultures, topical antimicrobials, and when ordered, systemic antibiotics. Report new odor, warmth, increased drainage, fever, or pain spikes immediately.
Dressings manage moisture. Skin heals best when the wound bed stays moist, not soggy. There is no one best dressing for stage 4 pressure ulcer in every case; dressings change as the wound changes. If surrounding skin looks waterlogged or irritated, it may be time to switch.
Advanced therapies when appropriate. A wound VAC for stage 4 pressure ulcer (negative pressure wound therapy) can remove exudate and encourage tissue growth in the right patients. For large or complicated wounds, surgical consults and grafts may be considered once infection and nutrition are optimized.
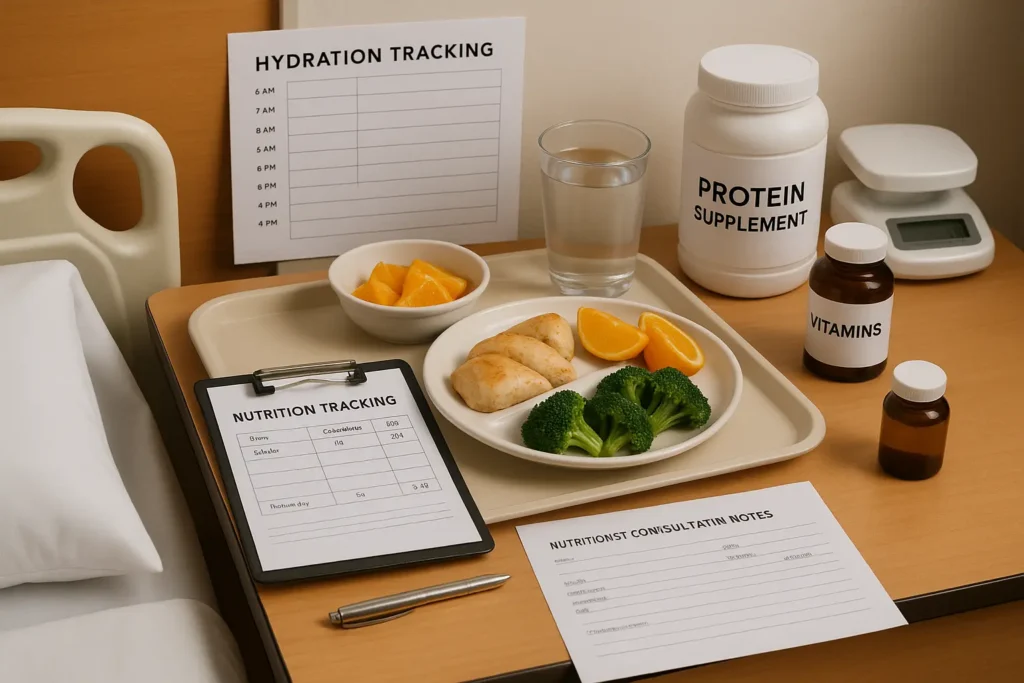
Nutrition fuels healing. Advanced wounds increase calorie and protein needs. A dietitian consult should be part of the care plan. Track what’s actually eaten and share concerns early.
Pain control and dignity. Dressing changes can hurt. Pre medication, gentle handling, and explaining each step reduce trauma and build trust.
How long does a Stage 4 bedsore take to heal?
There is no single timeline. Stage 4 pressure ulcer healing time depends on wound size and depth, infection status and speed of treatment, circulation and other conditions (like diabetes), nutrition and hydration, and crucially, how consistently the team offloads pressure and follows the plan. When a plan is working, families usually see steady signs: a cleaner wound bed, less slough, healthy red granulation, and stable or shrinking measurements over time. If weeks pass with little change, ask for a wound care specialist review.
Can a Stage 4 pressure ulcer heal?
Sometimes, yes. Many Stage 4 wounds improve, and some close fully, when offloading, debridement, infection control, dressings, and nutrition all work together. Healing isn’t guaranteed, and it often takes time. The care team should be honest about goals: full closure, partial closure, or maintenance, based on your loved one’s overall health.

What about “life expectancy” in Stage 4?
Searches for stage 4 bedsore life expectancy are common, and it’s understandable to worry. A Stage 4 wound signals serious risk, but it doesn’t determine the future by itself. Overall health, infections, mobility, nutrition, and the quality and consistency of care matter more. Ask the physician for a personalized outlook and consider a second opinion if you’re not satisfied with the answers.
Florida lens: when slow healing may signal a care problem
Florida facilities must meet state and federal standards of care. When families see repeated gaps (no reliable turning schedule, missed dressing changes, late specialist referrals, conflicting notes, weight loss without action), it’s reasonable to escalate. Start with the charge nurse and request a care plan conference. Keep a calm tone and keep records. If problems persist, we can arrange a confidential, no pressure legal review tailored to Florida cases.
One look reference
| Treatment focus | What to ask the team in Florida facilities |
|---|---|
| Offloading & support surfaces | “Show me the turning schedule and the mattress details; how is adherence documented each shift?” |
| Debridement & infection control | “What type of debridement are we using and why? Have we cultured the wound? What’s the plan if drainage/odor increases?” |
| Dressings & moisture | “Why this dressing now? How will you decide when to change it? How are you protecting the surrounding skin?” |
| Advanced therapies | “Would a wound VAC for stage 4 pressure ulcer help here? If not, what criteria would change that?” |
| Nutrition & pain | “Has a dietitian seen my loved one? What pain plan is in place before dressing changes?” |
About photos, diagrams, and privacy
Families often ask about bed sores stage 4 pictures or stage 4 pressure ulcer pictures. We avoid posting graphic galleries. If you track the wound for care plan meetings, do it respectfully: photograph at a consistent distance with a measuring scale, note pain and drainage in a private log, and store images securely. If you need visuals, ask the care team for non graphic staging diagrams or educational illustrations that explain depth and tissue layers without shocking content.
Special locations: sacrum and tailbone
A stage 4 sacral wound is common because the area bears pressure when a person sits or lies on the back. You may hear older terms like stage 4 decubitus ulcer in records; it means the same stage of pressure injury. Location can change the dressing approach and offloading strategy, so ask how positioning will protect that specific site.
A simple plan families can follow this week
In Florida facilities, small daily actions tend to drive the biggest gains. Read the plan, attend the first dressing change if possible, and write down what you see. Confirm the turning schedule and who is responsible on each shift. Track food and fluids, not just what’s offered. If progress stalls, request a wound care consult and a plan review. If concerns keep piling up, we can walk you through a free, confidential case review so you understand your options without pressure.
Soft next step for Florida families
Worried that care gaps are slowing healing? Share your notes and photos with us privately. We’ll explain how Florida cases typically move forward and whether a legal investigation makes sense for your family. No obligation, no upfront cost.