Quick note before we begin This is general information for Florida families. It isn’t medical or legal advice. If your loved one has a worsening wound, fever, confusion, or severe pain, call the care team or 911.
Table of Contents
Why advanced bed sores often signal neglect
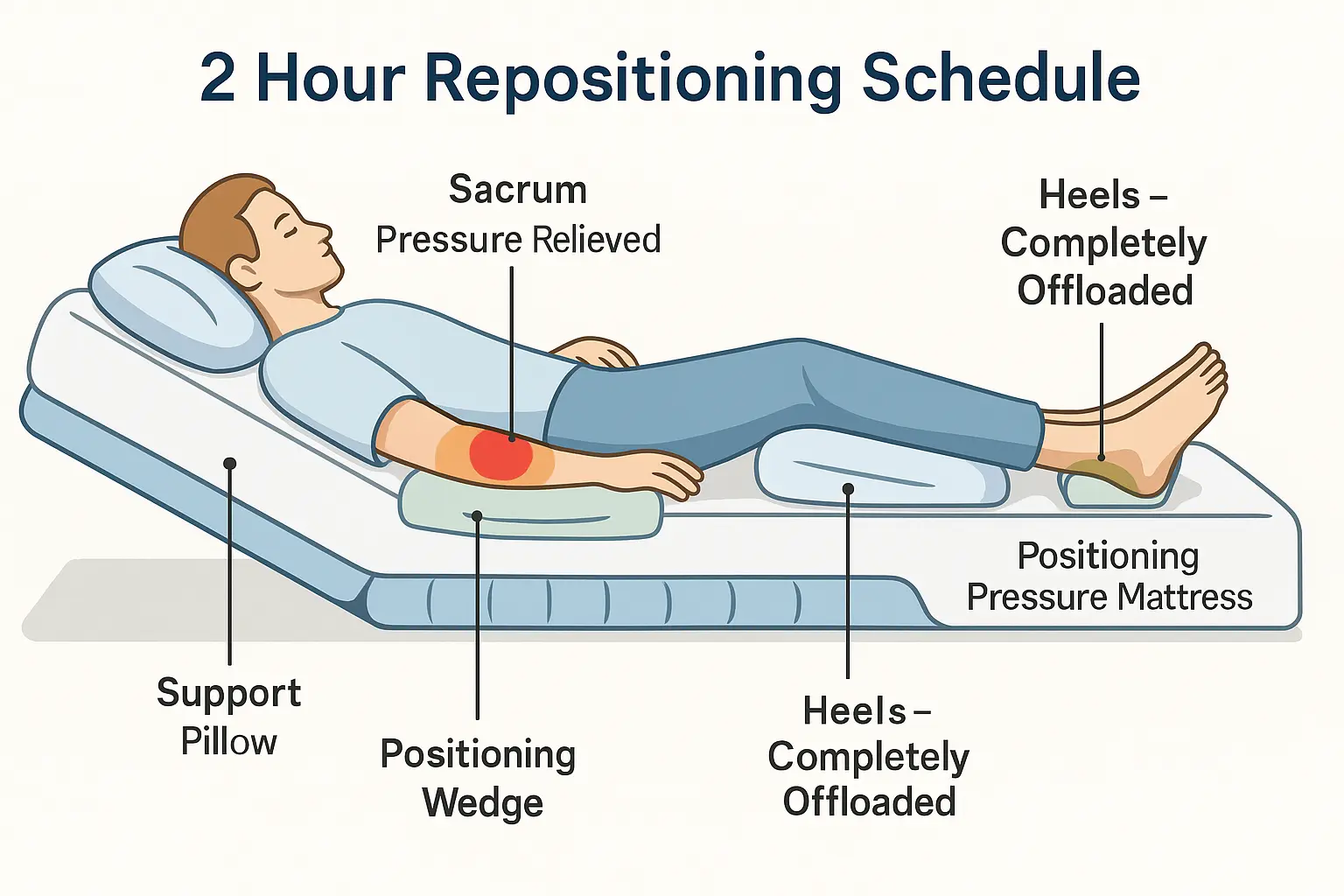
In a well run Florida nursing home, staff prevent pressure injuries with routine turning, true offloading, moisture and skin care, nutrition support, and speedy referrals when a wound appears. Stage 3 and Stage 4 bed sores rarely appear overnight; they build when small gaps become big ones. A missed turning schedule here, a delayed dressing change there, and an overlooked dietitian consult, soon a shallow wound deepens, bioburden rises, and tissue fails.
Neglect can be intentional or systemic. Short staffing, poor training, and weak documentation often hide the story. That’s exactly why families who suspect neglect should move quickly to preserve records and request a formal care plan meeting. The care plan is your map; when the facility doesn’t follow it, or keeps changing it without explanation, risk rises.
Can you sue a nursing home for bed sores?
Yes, if negligence caused the pressure injury or made it worse. In Florida, claims often proceed under residents’ rights and negligence theories, and in some cases overlap with medical negligence. A medical malpractice lawyer will look for a duty of care, a breach of that duty, a causal link to the injury, and damages. That sounds technical; in practice, it’s simpler: what should have been done, what wasn’t done, and how did the resident suffer because of it?
Families don’t need to prove the whole case on day one. They do need to act. Preserve photos, request records, and ask for all turning logs, wound assessments, physician orders, dietitian notes, and any wound care consults. The sooner you start, the easier it is for counsel to secure the evidence.
Red flags vs reasonable explanations (to guide your next conversation)
Use this as a conversation tool with the DON, wound care nurse, or administrator.
| If you’re seeing… | What the facility should be ready to show you… |
|---|---|
| “We’re short today,” yet your loved one sits on the wound for hours. | A turning/offloading schedule that matches charting and your observations, plus proof of pressure relief surfaces actually in use. |
| A Stage 2 ulcer that becomes Stage 3 or 4 over weeks. | Timely wound care referrals, debridement orders, dressing changes as ordered, cultures if indicated, and a documented reason for any delay. |
| Repeated maceration or foul odor. | Moisture balance plan changes, perineal skin care protocol, and culture/antimicrobial decisions noted by the provider. |
| Weight loss or poor intake alongside slow healing. | Dietitian assessments, protein/calorie goals, and interventions (supplements, feeding assistance) actually delivered, not just ordered. |
| Copy paste charting that doesn’t match reality. | Consistent, specific nursing notes, not identical blocks of text; incident reports when care variances occur. |
Bed sore Stage 4 treatment, why it matters legally
Treatment is a medical issue, and a legal one. Florida juries and insurers look at whether staff implemented stage appropriate care: real offloading every shift, timely debridement, documented infection control, moisture balanced dressings, adequate nutrition and hydration, and referrals to wound specialists when progress stalls. When bed sore stage 4 treatment falls short of accepted standards and harm follows, legal exposure grows.
If your loved one is on the sacrum or buttocks for long stretches, ask who approved the schedule and why. If a wound VAC was indicated but never considered, ask for that rationale in writing. If the wound keeps deepening, push for a specialist consult and root cause review.
How pressure sore lawyers secure legal rights and recourse for bed sore victims
A Florida pressure sore lawyer translates your concerns into an evidence based case. The team will request and analyze the complete chart, staffing and assignment sheets, wound photos and measurements, device and equipment logs, dietary records, and transfer or hospital records. They often retain experts: wound care nurses, geriatricians, plastic surgeons, to compare the facility’s actions to what competent care required.
On damages, counsel documents pain, infection, sepsis risk, surgeries and hospitalizations, loss of mobility, and changes in life expectancy. If the facility ignored obvious risks or falsified records, that conduct affects the approach and potential exposure.
Stage 4 bedsore lawsuit settlement amounts: what drives value
There’s no honest one size figure. Settlement value in Florida depends on the injury’s severity and duration, complications like osteomyelitis or sepsis, the resident’s baseline health and independence, medical costs, future care needs, and the quality of the facility’s conduct and documentation. Cases involving delayed treatment, repeated missed turns, or altered records may command higher value. Your attorney will also consider venue, insurer posture, and how a jury is likely to view the timeline.
Be cautious with online “averages.” Strong cases are built, not guessed. A free evaluation gives you a tailored sense of range without committing you to anything.
What to do for bed sores right now (Florida)
Start with safety. Ask the charge nurse to walk you through the current care plan: offloading schedule, surface selection, dressing type and frequency, pain management, and when the next provider visit occurs. If progress has stalled, request a wound care consult and a formal care plan meeting that includes nursing leadership and the attending provider. If your loved one isn’t safe where they are, discuss transfer options.
Document respectfully and consistently. Use a wound ruler in each photo, keep the distance the same, and note date, drainage, odor, and pain behaviors. Store images securely. Summarize each day’s turning and dressing activity in a short note to yourself; those details help your legal team confirm gaps.
You can also contact the Florida Long Term Care Ombudsman Program to register concerns while you explore legal options. A complaint does not replace a civil claim, but it creates an external record.
Evidence that moves cases faster
Pack this into a single folder so counsel can act quickly.
| Evidence to gather | Why it matters in Florida cases |
|---|---|
| The complete medical chart, including wound assessments, MAR/TAR, flow sheets, and care plans. | Shows what was ordered, what happened, and when the team escalated (or didn’t). |
| Turning/offloading logs and assignment sheets. | Connects staffing and workload to missed turns and late care. |
| Dietitian notes, weekly weights, intake records. | Links nutrition to healing; flags preventable failures. |
| Photos with dates and measurements. | Builds an objective timeline of staging and progress. |
| Hospital/ER records after transfers. | Independent documentation often corroborates problems. |
“What is the fastest way to get rid of bedsores?”
There isn’t a magic shortcut. The fastest path is the right path: reliable offloading every shift, the correct dressing and moisture balance, prompt debridement when ordered, infection control, and enough calories and protein to heal. Families accelerate this by verifying the plan, observing whether staff follow it, and pushing for specialist consults when progress stalls.
How to treat pressure sores on buttocks, what families can push for
Buttock and sacral ulcers demand true pressure relief, not just “reposition as tolerated.” Ask for a surface that matches risk level, such as a high quality pressure redistribution mattress or cushion, and confirm that incontinence care protects surrounding skin. Treatment should evolve as the wound changes. It’s reasonable to ask the nurse to explain why a specific dressing is in use today, when it will be reassessed, and how pain will be managed around changes.
Families should also confirm that providers have ruled out or treated infection and consulted wound specialists for Stage 3 or 4 ulcers. When answers feel vague, write down your question and request a written response for the chart. Clear records serve your loved one’s health and your legal rights.
Can you sue, and should you?
If neglect caused an advanced ulcer, you can sue a nursing home for bed sores in Florida. Whether you should sue is personal. Many families file to secure future care, hold a facility accountable, and deter repeat conduct. A free, confidential review can help you weigh options without pressure.
FAQs
Can you sue a nursing home for bed sores in Florida? Yes, when substandard care causes an ulcer or allows it to worsen. A lawyer will evaluate records, staffing, and wound care timelines to confirm negligence and damages.
What are my legal rights and recourse for bed sore victims? You may seek compensation for medical treatment, pain and suffering, and related losses. Pressure sore lawyers use expert reviews and complete facility records to pursue accountability and safer care.
Does Stage 4 bed sore treatment affect my case? It often does. Courts and insurers look at whether accepted bed sore Stage 4 treatment steps were timely and consistent, including offloading, debridement, infection control, and nutrition.
How are Stage 4 bedsore lawsuit settlement amounts determined? By the injury’s severity, complications, care failures, documentation quality, and impact on life and costs. A free review gives you an individualized sense of range.
What should I do for bed sores right now? Escalate care, insist on a documented plan, photograph the wound with measurements, request specialist consults, and get a Florida legal review to protect your options.
Next step for Florida families
If you want a second set of eyes on the charting and your photos, we can review them confidentially and explain typical paths forward in Florida. There’s no cost to learn your options, and no obligation to hire anyone.