Important: This page is general information for families. It isn’t medical advice. If your loved one has new fever, confusion, worsening breathing, or declining responsiveness, seek medical care immediately.
Table of Contents
What is anoxic brain injury?
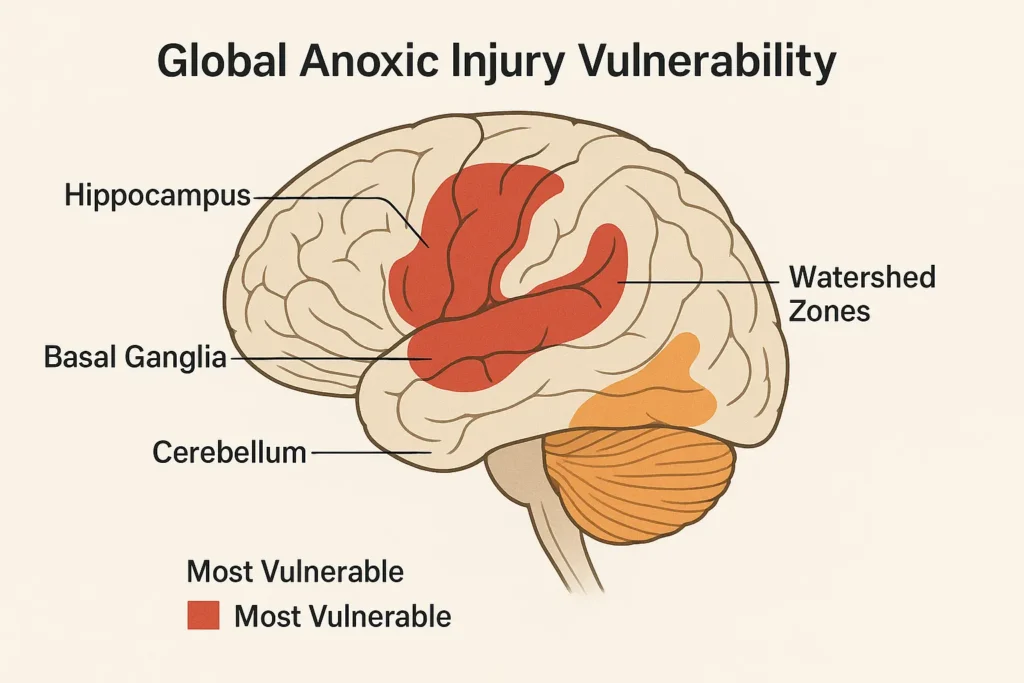
Anoxic brain injury happens when the brain is starved of oxygen; “hypoxic ischemic” injuries include both low oxygen and poor blood flow, such as after cardiac arrest, near drowning, or choking. Brain cells are highly sensitive to oxygen loss and injury can begin within minutes, which is why rapid resuscitation and early critical care matter so much.
Anoxic brain injury symptoms (and how they change)
Early symptoms often reflect diffuse, “global” injury: reduced responsiveness or coma, disorientation, memory and attention problems, slowed thinking, agitation, balance and coordination issues, and changes in mood or behavior. In the weeks that follow, families may notice fatigue, headaches, sensory sensitivity, sleep disruption, and executive function challenges that make daily activities hard. Severity ranges widely; some people improve to independent living, while others need long term support.
Anoxic brain injury recovery stages
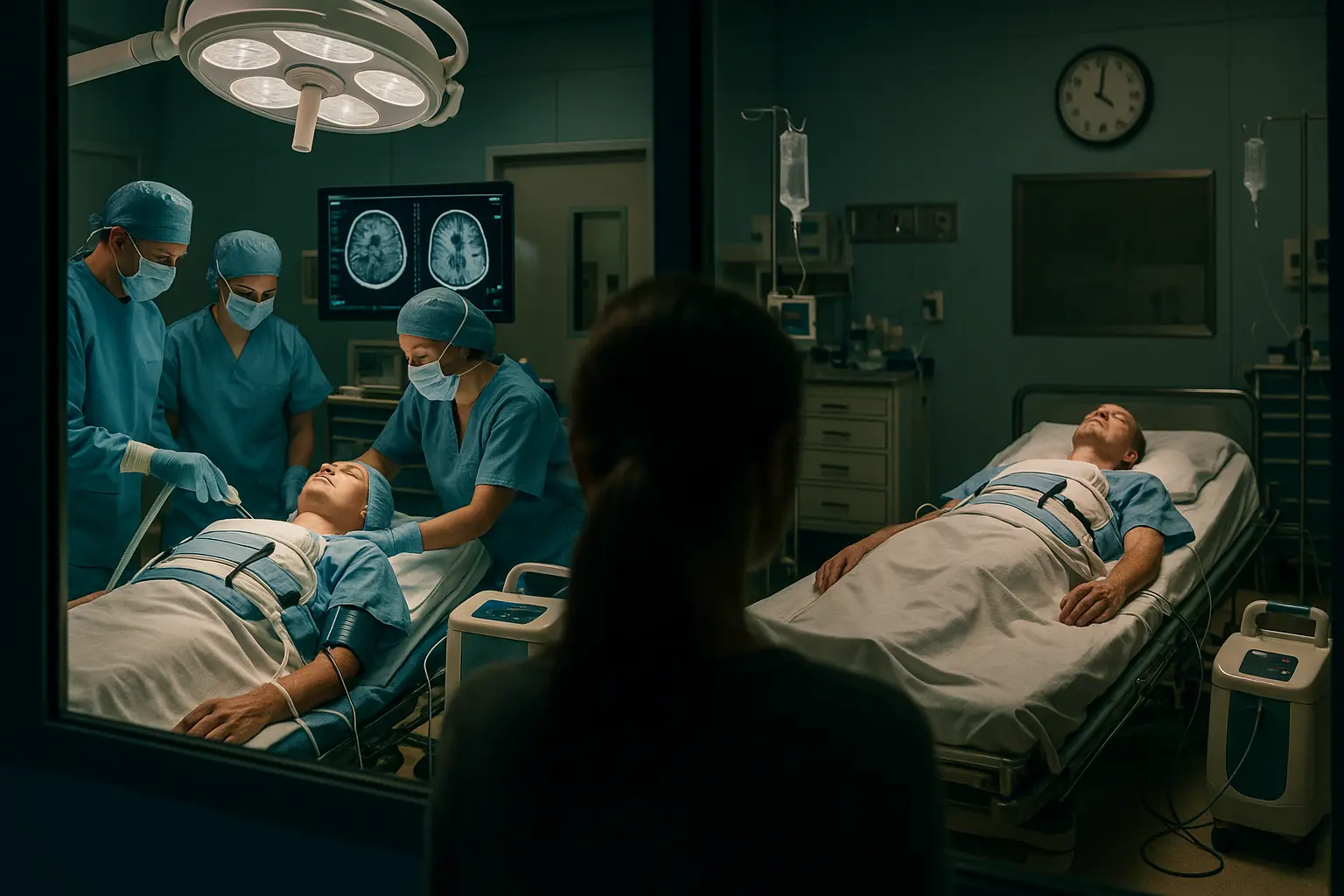
Hospitals and rehab teams don’t rely on one “magic number.” They track progress with repeated neurological exams and validated scales, then adjust therapy as cognition and mobility return. After cardiac arrest, modern guidelines recommend waiting days and using a multimodal approach (exam, EEG, imaging, blood markers) before predicting long term outcome; this helps avoid premature, overly pessimistic decisions.
Anoxic brain injury recovery timeline
Recovery unfolds over phases rather than a fixed stopwatch. The fastest changes usually appear in the early months after injury as swelling resolves and the brain “re organizes.” Improvements can continue with therapy as the nervous system adapts (neuroplasticity), even when progress seems to slow. Families commonly describe plateaus followed by smaller but meaningful gains: better attention, more consistent speech, improved walking endurance, which add up over time.

The journey (Florida care settings)
| Phase in Florida care | What you can expect & what moves recovery forward |
|---|---|
| ICU / acute hospital (days to weeks) | Stabilization after oxygen loss, ventilation, seizure monitoring, infection control. Teams watch for return of consciousness and purposeful responses, then start gentle therapies at bedside. Families help by orienting the patient (name, place, date), supporting sleep/wake cycles, and asking how pain, sedation, and delirium are managed. |
| Inpatient & outpatient neuro rehab (weeks to months, sometimes longer) | Daily PT/OT/speech therapy to rebuild attention, memory, mobility, swallowing, and self care. The plan evolves with energy limits and cognition. Case managers coordinate home services, equipment, and caregiver training. In Florida, ask about specialized neuro rehab programs and community re entry resources; document goals every 2 to 4 weeks so gains are visible and insurance authorizations stay current. |
Can you recover from an anoxic brain injury?
Yes, many people do, especially when early medical stabilization is followed by consistent, individualized rehabilitation. Recovery potential depends on how long oxygen was lost, how quickly effective CPR and advanced care began, age and health before the event, and complications like infection or seizures. The pattern isn’t all or nothing; partial recoveries can still restore communication, mobility, and meaningful independence.
Anoxic brain injury recovery timeline vs. expectations
Families often ask for a calendar. A more helpful frame is trend: Is responsiveness increasing? Is attention lasting longer? Are therapy goals advancing? When trends stall, teams reassess pain control, sleep, nutrition, mood, and medical complications that quietly drain progress. Neuroplasticity supports learning and re learning skills well beyond the early months, which is why purposeful practice, and rest, both matter.
Anoxic brain injury prognosis (and what “severe” means)
“Severe anoxic brain injury” usually refers to deep, prolonged unconsciousness, limited purposeful movement, and extensive MRI changes. Even then, outcome can vary. Best practice is to combine bedside exam with EEG, MRI/CT, and lab markers over time; confirming prognosis too early risks error. Families should hear a clear plan for when and how clinicians will re evaluate, and what specific signs would change the outlook.
Life expectancy after an anoxic brain injury
There isn’t a single number. Long term survival depends on the injury’s severity, medical stability (breathing, swallowing, infection control), co existing heart and lung disease, and the safety and consistency of daily care. People with milder injuries often live full lives; those with complex medical needs face higher risks related to infections, aspiration, and immobility. Your treating physician can best translate clinical details into individualized life expectancy guidance; beware of generic internet charts that ignore your loved one’s specific condition.
Real options that move the needle
Start with a written rehab plan that matches current abilities and energy limits. Ask for measurable goals (e.g., 10 minutes of sustained attention; 5 safe transfers per day), then track practice and rest. Confirm insurance authorizations early and appeal denials with therapy notes that show new gains. In Florida, explore specialized neuro rehab programs and caregiver training through major hospital systems and statewide brain injury resources; a social worker or case manager can connect you. If oxygen loss occurred in a Florida facility and you suspect delayed response, equipment failure, or medication error, you can request records and a timeline review; our team can provide a no cost legal consult to explain options.

Hyperbaric oxygen therapy for anoxic brain injury
You may see stories about “miraculous recovery from an anoxic brain injury” after hyperbaric oxygen therapy. Hyperbaric medicine has approved, specific indications (for example, carbon monoxide poisoning), but routine use for chronic anoxic brain injury is not established in major guidelines. If you’re considering HBOT, discuss potential risks, costs, and realistic benefit with your treating physician, and ask how progress would be measured.
What to watch for and why it matters
| Red flag | Why it matters | Next step in Florida |
|---|---|---|
| New fever, labored breathing, confusion, or decreased responsiveness | Infection, pulmonary issues, or seizures can erase hard won gains if untreated | Call 911 or the care team; ask if emergency evaluation is needed |
| Sudden drop in therapy tolerance or new pain | Undiagnosed depression, sleep apnea, spasticity, or medication side effects often sap progress | Request medical review and therapy re assessment; adjust the plan |
| Weight loss or swallowing trouble | Malnutrition and aspiration risk increase complications | Ask for dietitian and speech language pathology evaluations |
| Care plan not documented or not followed | Inconsistent care slows recovery | Request a family team meeting; escalate through patient relations if needed |
Florida FAQs
What is an anoxic brain injury? It’s brain damage from lack of oxygen (often after cardiac arrest, choking, or near drowning). It can be mild to severe, and outcomes vary widely by person.
What are common anoxic brain injury symptoms? Early: reduced responsiveness, confusion, memory and attention problems. Later: fatigue, headaches, sensory sensitivity, sleep and mood changes, and slowed thinking.
What does the anoxic brain injury recovery timeline look like? Fastest gains usually appear in the early months; progress can continue with focused therapy over longer periods, often in smaller steps that still improve daily life.
Can you recover from an anoxic brain injury? Many people do, especially with early stabilization and sustained rehab. Recovery spans a spectrum, from partial to substantial independence, based on injury severity and complications.
Is hyperbaric oxygen therapy recommended for anoxic brain injury? Hyperbaric oxygen has specific, approved indications; routine use for chronic anoxic brain injury isn’t established in major guidelines. Discuss risks and goals with your physician before pursuing it.
Next steps
Build a simple binder: contacts, medications, therapy goals, and a daily log of sleep, nutrition, and practice. Tour at least one inpatient rehab and one outpatient program; pick the team that speaks in goals you understand. If the injury stemmed from a Florida hospital, EMS, pool, or nursing home event and you suspect negligence, ask for records in writing and note who you spoke with and when. Our Florida team can review your timeline, records, and photos without cost or obligation and explain your options in clear English or Spanish.